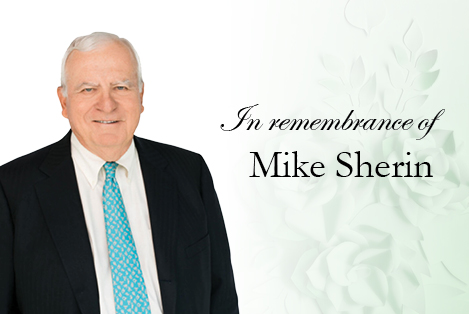
A tribute to Mike Sherin








JND named #1 Claims Administrator in the U.S.
JND Practice Areas
We deliver the most reliable and comprehensive legal administrative resources and services available to our clients.
Class Action
Our team has handled some of the most complex class action settlements in the country's history.
eDiscovery
We leverage a comprehensive and flexible cloud-based platform to meet even the most complex litigation management needs.
Government Services
JND has proved its ability to understand and address the unique needs of government entities throughout the United States.
Incident Response Services
JND’s comprehensive Incident Response Service comprises the expertise of our industry leading Legal Notice, Settlement Administration, and eDiscovery Solutions.
Legal Notice Programs
JND's Notice Experts have been providing consultation for years on all facets of Class Action settlements, including notice issues.
Learn More
We deliver the most responsive, trustworthy and technically superior results you will find.
Our Cases
JND and its principals and subsidiaries have handled a wide array of cases over the years. See below for a select sample of matters.
450
Million Claims Processed Since 2016
5
Billion Dollars in Distribution Since 2016
1100
Matters Won Since 2016
24
Hour Responsiveness
Latest News
JND Receives Hall of Fame Awards for End-to-End eDiscovery, Managed eDiscovery and Litigation Support Services in 2024
March 28, 2024The National Law Journal has presented JND eDiscovery with its 2024 Hall of Fame Award in the Best Managed eDiscovery & Litigation Support Provider and Best End-To-End eDiscovery Provider categories. JND also has also been ranked "Top 3" in those categories in the annual readers' poll eight times.
JND Legal Administration Named #1 Class Action Claims Administrator by The National Law Journal in 2024
March 26, 2024JND Legal Administration has again been named as the nation's #1 Class Action Claims Administrator by U.S. attorneys and legal service providers, as published in the 'Best of 2024' supplement to the National Law Journal. Additionally, the company has again been honored with a National Law Journal Hall of Fame Award for the third consecutive year.
Request a Proposal
If you are interested in any of our services, you can request a proposal by filling out the fields in this section.
CONTACT US
- Case Inquiry
- 1-800-207-7160
- info@JNDLA.com
- www.JNDLA.com
- Jen@JNDLA.com
- Neil@JNDLA.com
- David@JNDLA.com
- Careers@JNDLA.com
FOUNDING PARTNERS
JOIN US